What Does Measles Look Like?
Risk Factors for Increased Fatality
1. Age at infection: Measles can affect anyone, but young children under the age of 5 and adults older than 20 are at higher risk of complications and death from measles. Infants under and young children are at the highest risk of death from measles due to their undeveloped immune systems and waning maternal antibodies. This vulnerability is further exacerbated by failure to receive the vaccine's first dose at 12-15 months of age, leading to severe symptoms and complications like pneumonia and encephalitis, which can lead to death. Young children aged one to four are particularly vulnerable due to not completing their vaccination series and their still-developing immune systems. Adults over 20 years are also at increased risk of severe complications and death if unvaccinated as youngsters. those with background health conditions and weakened immune systems may experience severe symptoms later in life
2. Malnutrition: Malnutrition weakens the immune system's response to infectious diseases like measles, making individuals more susceptible to severe illness and complications. Essential nutrients like vitamins A, C, D, protein, and zinc are crucial for maintaining immune function. Deficiency in these nutrients can impair the body's ability to produce antibodies and fight off the virus, making individuals more susceptible to severe illness. Additionally, malnutrition can affect respiratory function, making them more susceptible to respiratory infections like pneumonia. Inadequate intake of essential nutrients can also prolong illness duration and delay recovery. Malnourished individuals with pre-existing health conditions may have compromised immune systems and reduced resilience to severe illness. Undernourished children, especially those living in resource-poor settings, are at heightened risk of experiencing complications such as severe pneumonia and diarrhea, which can significantly increase the risk of death.
3. Immunosuppression: Severe measles consequences, such as pneumonia and encephalitis, are more common in those with compromised immune systems, such as those receiving chemotherapy, organ transplant patients, or those with HIV/AIDS, cancer, or autoimmune illnesses. This vulnerability is especially noticeable in patients receiving immunosuppressive treatment for autoimmune disorders or following an organ transplant. These people might also have trouble getting rid of the virus, which raises the possibility of spreading it to others.
4. Lack of vaccine: Unvaccinated people do not have the immunity to defend themselves against the measles virus, which makes the disease very contagious. When they come into contact with an infected individual, they have a higher chance of catching the virus, which can cause serious sickness and even death in some cases. The best defense against measles is vaccination. The measles vaccine offers lifelong protection against the virus. It is typically given as part of the measles-mumps-rubella (MMR) vaccination series between 12-15 months of life. Emergencies of measles can burden healthcare systems and cause delays in diagnosis, treatment, and supportive care when vaccination rates drop below herd immunity.
5. Access to healthcare: Limited access to healthcare services can delay the diagnosis and treatment of measles, increasing the risk of complications and death. In many low-resource settings, healthcare facilities may need more staffed and equipped to handle the influx of measles cases during outbreaks. This can result in delays in seeking medical care, inadequate treatment, and poor outcomes for patients, particularly those with severe complications such as pneumonia and encephalitis.
6. Secondary Infections: Measles weakens the immune system, making individuals more susceptible to secondary bacterial and viral infections. Complications such as pneumonia, otitis media (ear infection), and gastroenteritis can occur concurrently with measles or develop due to the virus's impact on the body's defenses. Secondary infections can significantly increase the risk of death, particularly in cases where prompt medical intervention is unavailable or delayed.
7. Overcrowded Living Conditions: Measles spreads rapidly in crowded environments, such as refugee camps, urban slums, and densely populated areas. Overcrowding facilitates the transmission of the virus from person to person, leading to large outbreaks with high rates of morbidity and mortality. In such settings, individuals may have limited access to healthcare, sanitation, and adequate nutrition, further exacerbating the risk of severe illness and death from measles.
8. Type and severity of complications: Measles can lead to serious complications such as pneumonia, encephalitis, and SSPE. Pneumonia is common in young children and those with weakened immune systems, while encephalitis can cause seizures, coma, and permanent neurological damage. SSPE is a rare but fatal complication resulting from persistent measles virus infection in the brain. Dehydration, especially in young children, can lead to organ failure and death. Malnutrition also increases the risk of severe complications and death. Secondary infections, such as sepsis or respiratory infections, can be life-threatening if not treated promptly.
Pathogenesis of Measle
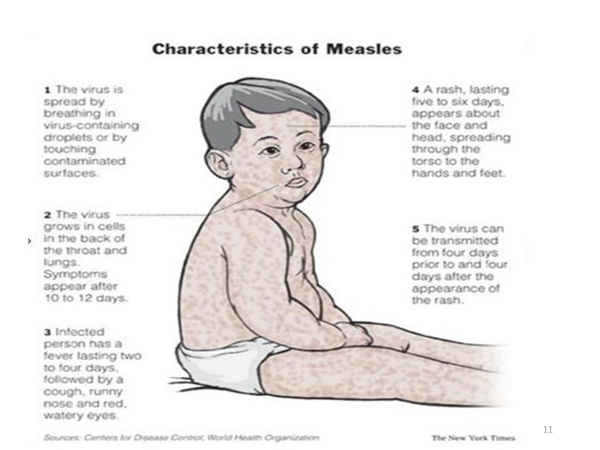
Respiratory droplets from an infected person's cough, sneeze, or speech are the main ways to spread measles. The main location of infection is the nasopharynx and respiratory epithelium. The virus spreads to local lymph nodes, where it infects and multiplies. A primary viremia develops after two or three days of invasion and replication in the pulmonary epithelium and regional lymph nodes, which spreads to the reticuloendothelial system. A secondary viremia spreads the virus to body surfaces and is associated with epithelial necrosis and giant cell formation in body tissues. This occurs 5-7 days after the initial infection. Virus shedding begins in the prodromal phase. With the onset of the rash, antibody production begins, and viral replication and symptoms start to subside. The Measles virus also infects CD4+ T cells, causing suppression of the immune response.
Clinical Features
Incubation period: This phase lasts on average 10 – 12 days from exposure to the prodromal phase and 14 days from exposure to the onset of rash but may vary from 7 – 14.
prodromal period: Last 2 – 4 days (but may vary from 1 – 7 days) and is characterized by a high continuous fever (40 degrees), anorexia, cough, conjunctivitis, and coryza known as the three "C"s.
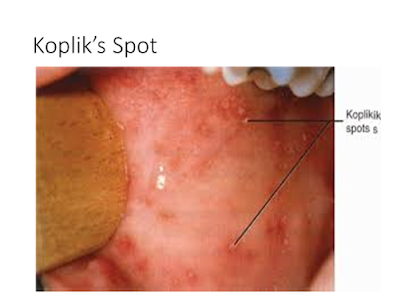
Appearance of the rash: first is the Koplik’s spots at the mucous membrane of the lips. The condition manifests as punctate blue-white patches on the bright red surface of the buccal mucosa, and it happens 1-2 days before to 1-2 days after the rash appears. They are pathognomonic for measles.
The maculopapular eruption resulting from measles infection lasts 5-6 days. It starts at the hairline and spreads to the upper neck and face. Gradually, it proceeds downward and outward, reaching the hands and feet. The maculopapular lesions are generally discrete but may become confluent, particularly on the upper body. Initially, lesions blanch with fingertip pressure. By 3–4 days, most do not blanch with pressure. Fine desquamation occurs over more severely involved areas. The rash fades in the same order it appears, from head to extremities. The child then begins to get better. Other symptoms may include photophobia, periorbital edema, myalgia, runny nose, and sore throat.
Hemorrhagic measles: high fever, seizures, delirium, respiratory distress, bleeding into the skin and mucous membrane.
Inapparent measles: asymptomatic or mild symptoms, provide boost measle ab titers which protect against future infection.
Atypical: measle infection among those vaccinated with killed virus vaccine but not immunized. Mild fever, headache, abdominal pain, and myalgia precede a rash.
Diagnoses and Differentials
Measles infections are mostly diagnosed clinically, with a complete history and physical examination. Pay attention to evidence of severe diseases like inability to feed or breastfeed, convulsions, corneal clouding, extensive mouth ulcers, stridor, dehydration, and severe malnutrition. The differential diagnoses of measle infection include the following:
- Other exanthematous immune-mediated illnesses include rubella, adenoviruses, enteroviruses, and Epstein-Barr viruses.
- Exanthem subitem (HHV-6) and erythema infectiosum may also be confused with measles.
- Mycoplasma pneumoniae and group A streptococcus may also produce rashes similar to measles.
- Kawasaki syndrome can manifest many of the same findings as measles. Sometimes, drug eruptions are misdiagnosed as measles.
Treatment of measles
Treatment is mainly supportive. There is no need for treatment for uncomplicated measles infection. Adequate hydration, oxygenation, and comfort are goals of therapy. Gamma globulin is of little value.
- Patients need to be monitored for the emergence of bacterial infections, which should be treated with the right antibiotics.
- Give vitamin A for three days at 100,000–200,000 IU.
- Maintain bed rest.
- If there is sensitivity to light, keep the room dark.
- Clean and remove eye secretions with warm saline or water.
- Encourage the patient not to rub the eyes.
- Administer, antipyretic medication and tepid sponge baths as ordered.
- You can use a cold mist vaporizer to help with cough relief.
- Apply antipruritic medication to prevent itching.
- Isolate the child until the fifth day of the rash
Dosage of Vitamin A
- 50 000 IU for a child aged < 6 months,
- 100 000 IU (6–11 months) or
- 200 000 IU (1–5 years).
If there is any eye sign of vitamin A deficiency, give a third dose 2–4 weeks after the second dose on follow-up.
Complications of Measles
1. Respiratory
- Pneumonia, otitis media
- Croup, Bronchiolitis
- Pneumothorax
- Emphysema
- TB
2. CNS
- Seizures
- Encephalitis
- SSPE (Subacute Sclerosing Panencephalitis)
3. GIT
- Diarrhea/vomiting
- Cancrum oris
- Lactose intolerance
- PEM (Protein Energy Malnutrition)
4. Ocular ( due to Vit A deficiency)
- Corneal opacity/ulceration
- Blindness
5. Hematological
- Thrombocytopenia
- DIC
Prevention of Measles
The measles vaccine has been in use since the 1960s. It is safe, effective, and inexpensive. Presently a live attenuated vaccine is used alone or in combination with other MMRV. In 2010, the World Health Assembly (WHA) identified three milestones for measles control by 2015.
- Increased routine coverage with the first dose of MCV to ≥90% nationally and ≥80% in every district.
- Reduction in global annual measles incidence to <5 cases per million population.
- Reduction in global measles mortality by 95% from the 2000 estimate.
The herd protection threshold for measles is the highest for all VPD ranging from 89-94%. In 2015, the estimated worldwide coverage of 1st dose of measles vaccine was 85%. Despite the spread use of the measles virus worldwide, measles remains an important cause of death. Of the projected 20.8 million babies who were not given the first dosage in 2015, almost 50% come from India(3.2), Nigeria (3.0), Pakistan (2.0), Indonesia(1.5), and Ethiopia (0.7).
Contraindications
- Absolute contraindications include known hypersensitivity, severe malnutrition, and pregnant women.
- Relative contraindications include febrile illness, stable HIV patients, and TB patients.




This is well simplified ma. Thank you
ReplyDelete